Cornea and External Diseases Care
Fort Worth Cornea & External Disease Treatments
Meet Our Cornea Specialist
Ophthalmology Associates is proud to announce the addition of Dr. Sandy Iyer to our lists of highly specialized eye care professionals. Dr. Iyer’s field of expertise, Cornea and External Diseases and Cataracts, has broadened the eye care services we now offer at Ophthalmology Associates to include Corneal Diseases and Transplants, in conjunction with the cataract, glaucoma, retina and other eye care specialties already offered to our patients.
She has traveled, taught, and practiced all over the world. Dr. Iyer brings a unique perspective to Ophthalmology due to her extensive training and experience in different continents and healthcare economies. Dr. Iyer is excited to move to Fort Worth and become an active member of the medical communities of Tarrant and Hood counties. She is currently seeing patients in both Fort Worth and Granbury offices.
What are Corneal Diseases?

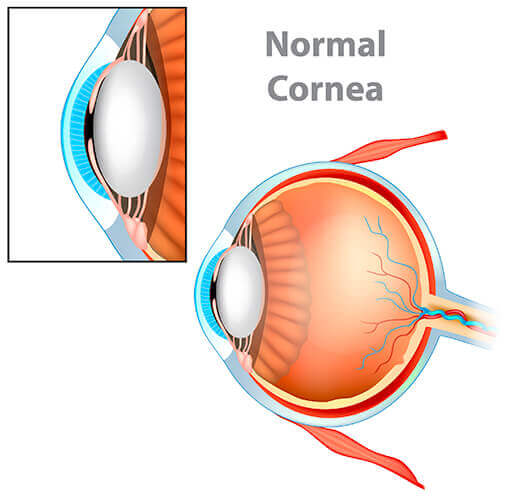
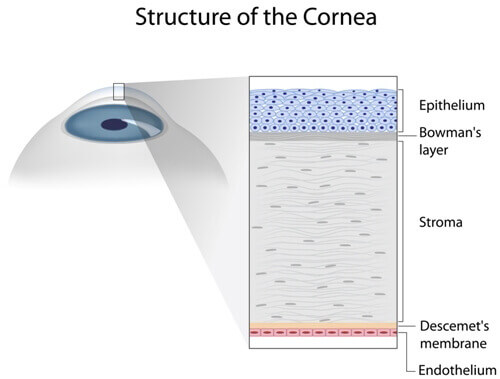
Cornea and external diseases involve the cornea and its many layers, the endothelial, iris, lens, the conjunctiva, and eyelids. The cornea can sustain damage through foreign objects, abrasions and infections, edema (swelling), and scarring.
The cornea can also be damaged through genetic or degenerative disorders. Conjunctivitis (pink eye), dry eye, keratoconus, pterygium, Fuchs’ Dystrophy, cataracts, nearsightedness, farsightedness, and astigmatism are a few of the maladies that can affect or injure the cornea and conjunctiva.
Timely and proper care by our Cornea Specialist, Dr. Sandy Iyer, can ensure the health of your cornea and vision.
What is Fuchs’ Dystrophy?
Fuchs’ Corneal Dystrophy is an inherited disease of the cornea causing cells of the corneal layer to die. These cells when healthy pump fluid to the cornea keeping it nice and clear. As the cells die fluid builds up, vision becomes cloudy and the cornea swells and becomes thick and puffy – (corneal edema).
What are the Symptoms of Fuchs’ Dystrophy?
Patients with early Fuchs’ may notice haziness in the morning which clears throughout the day caused by the moisture in your eyes from sleep drying normally through the day. As the dystrophy worsens, your vision becomes continuously blurred, you may experience a sensitivity to light and glare and a sandy or gritty feeling in your eyes.
How do you Treat Fuchs’ Dystrophy?
Fuchs’ cannot be cured. You may be able to control your vision problems with certain medications or eye drops to lessen the swelling of the cells in the cornea.
In cases of advanced corneal edema, a corneal transplant may be indicated. Dr. Iyer will discuss what treatment options are available after careful examination of your cornea. Corneal transplants have excellent success rates.
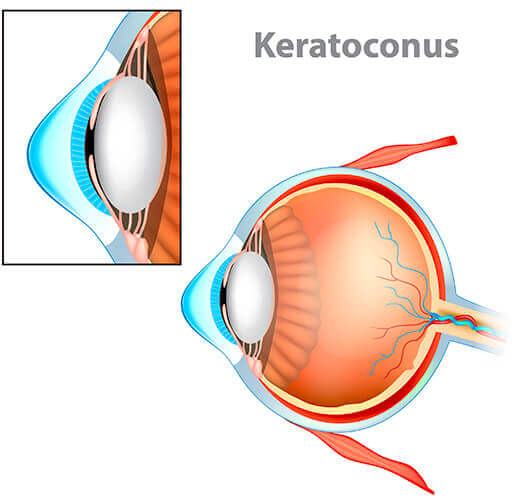
What is Keratoconus?
Keratoconus, pronounced KEHR-uh-toh-KOH-nus, develops when the cornea thins and forms a cone-shaped bulge of the cornea. This can result in blurry or distorted vision due to the distortion of the light entering the eye.
Herpes Simplex Virus
There are two types of herpes simplex virus that affect the eyes commonly known as Type I (HSV I) and Type II (HSVII). Type I, the most common, is the same virus that causes cold sores and fever blisters and the viral infection can be caused by touching a cold sore and then touching or rubbing your eyes.
Type II is spread through sexual contact. The infection once spread to the eye can spread deeper into the cornea causing redness and swelling and possibly the scarring of the cornea or ulcers on the cornea.
How do you Treat Ocular Herpes?
There is no cure for ocular herpes. Once you have the virus, it remains in your body, but mild cases can often be controlled with antiviral pills and/or steroid drops.
Your ophthalmologist may also scrape diseased cells from your cornea to help improve vision. If your cornea is scarred from a severe infection you may require a corneal transplant. Dr. Iyer will discuss all options with you after a thorough exam.
Corneal Ulcers
Bacterial, viral, fungal, and parasitic infections can occur when not exercising proper contact lens care, or failure to use protective eyewear at work or play. Corneal ulcers (open sores on the cornea) can result in these eye infections. Severe dry eye, eyelid disorders, or contact lens misuse can cause ulcers as well.
How do you Treat Corneal Ulcers?
Antibiotic, antiviral or antifungal eye drops are the first line of treatment. Undiagnosed ulcers can also result in scarring of the cornea which may lead to surgical intervention.
See your ophthalmologist at the first signs of pain or redness in the eye, severe pain or soreness, swelling of the eyelids, pus or discharge from the eye or white spots developing on your cornea. Do not try to self-medicate with over the counter drops unless directed by a physician.
Punctal Plugs
Punctal plugs are tiny devices inserted into tear ducts to block drainage thus increasing the eye’s tear film and moisture and may be used to treat “dry eye” symptoms and corneal disease associated with aqueous tear deficiency.
These “plugs” are no larger than a grain of rice and not harmful to living tissue. The procedure is performed in the office and takes very little time. Discomfort, side effects, and complications are very rare. Dr. Iyer will examine your eyes thoroughly to determine if punctal plugs are the best treatment option for you.
Conjunctivitis (Pink Eye)
Conjunctivitis, commonly called “pink eye” is the result of the conjunctiva becoming irritated by an infection, environmental irritants or allergies that cause swelling, itching, burning, and redness of the conjunctiva, (the protective membrane that lines the eyelids and covers exposed areas of the sclera, or white of the eye).
There are three main types of conjunctivitis: Viral, Bacterial, and Allergic. Some types of pink eye can be very contagious.
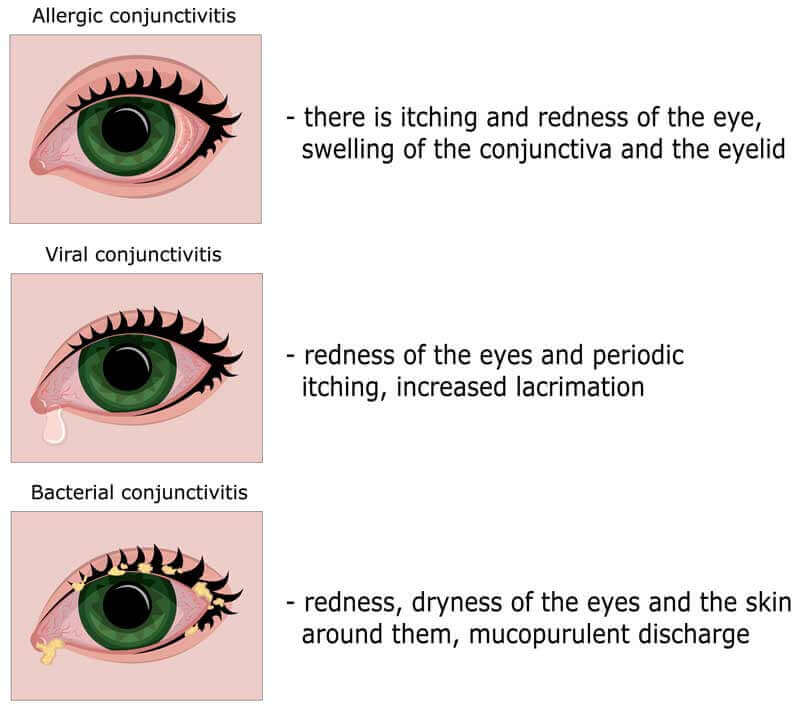
Conjunctivitis is usually painless and does not adversely affect vision. The infection will clear in most cases without requiring medical care. But for some forms of conjunctivitis, treatment will be needed. If treatment is delayed, the infection may worsen and cause corneal inflammation and a loss of vision. You should see your ophthalmologist if you are experiencing thick yellow discharge, pain in your eyes, or blurred vision.
Corneal Transplant
A cornea transplant, also known as keratoplasty, is performed when a patient’s cornea no longer allows light to enter the eye properly due to injury or disease, and vision is severely compromised. The goal of this procedure is to restore vision loss caused by the damaged cornea.
The cornea consists of multiple layers and transplants can involve any or all layers of the cornea. During this procedure, an eye surgeon removes part of your cornea and replaces it with corneal tissue provided by a human donor.
The donor tissue is obtained from an eye bank and is thoroughly screened before being accepted for transplantation.
Depending on the type of transplant performed and whether the transplant was performed along with other surgical procedures (like cataract surgery, glaucoma surgery, pupil repair, or retina surgery) the surgery is performed on an out-patient basis.
Eye drops help healing and prevents the risk of rejection. Healing time, success rates, and risks associated with transplants vary based on the type of transplant. When choosing Dr. Iyer you are choosing a highly trained surgeon who has extensive experience in these procedures. After a comprehensive exam of your condition, Dr. Iyer will fully discuss the best surgical options available for you.
Types of Cornea Transplant Surgery
There are several different types of cornea transplant surgeries.
Penetrating Keratoplasty (PK)
Penetrating Keratoplasty (PK) or Full Thickness transplant is performed when both the front and inner corneal layers are damaged. The donor cornea is then sewn into place. This type of procedure generally takes the longest time to regain complete vision (anywhere between 9-12 months or longer). Most patients will need glasses, contacts, or rigid gas permeable contacts after a transplant.
Deep Anterior Lamellar Keratoplasty (DALK)
Partial Thickness transplant involves the front and middle layers of the cornea and replaces it with a thin layer of donor tissue. This procedure has faster recovery time and rejection of donor tissue is lessened. This partial-thickness transplant can be repeated if necessary.
This procedure is used when necessary for patients with Keratoconus. Patients generally do very well after this type of transplant. The surgery is an outpatient surgery. Eye drops help healing and prevents the risk of rejection and infection.
Endothelial Keratoplasty (DMEK or DSEK)
In some patients, only the innermost layer or “endothelium” is damaged causing vision disturbance due to swelling. In this case, only the endothelium layer is replaced with donor tissue. There are two types of partial transplants. DSEK and DMEK.
The donor tissue for DSEK is thicker and typically easier to transplant and position. In DMEK, the donor tissue is thinner with a faster recovery time but more difficult to transplant. Dr. Iyer will choose and discuss the best surgical options based on your cornea’s condition.

